How to Submit a Corrected Claim
It may be necessary to submit a corrected claim when the original claim was submitted with incomplete or inaccurate information, such as an incorrect procedure code, date of service, or diagnosis code. The preferred process for submitting a corrected claim is to use the 837 transaction for both professional and facility claims, using claim frequency code 7.
Incorrectly submitting a corrected claim as a new claim could result in a denial.
To submit a corrected claim electronically:
Use the HIPAA 837 standard claims transaction and include the following information:
- Frequency code of “7” in loop 2300, CLM05-3 segment to indicate a corrected/replacement of a previously processed claim. Use “8” to void a claim billed in error.
- The initial claim number (in loop 2300, REF01 must contain “F8” and REF02 must contain the claim number).
- A free-form note with an explanation for the corrected/replacement claim, in loop 2300 claim note as:
- For professional and dental claims, segment NTE01 must contain “ADD” and segment NTE02 must contain the note, for example: NTE*ADD*CORRECTED PROCEDURE CODE.
- For institutional claims, segment NTE01 must contain “UPI” and segment NTE02 must contain the note, for example: NTE*UPI*CORRECTED LAB CHARGES.
For additional information regarding electronic corrected, replacement, or voided claims, visit our Electronic Transactions and Claim Payer ID web page.
To submit a corrected paper claim:
- Submit it as a replacement claim, clearly marking the claim as a corrected claim. Failure to indicate that a claim is a corrected claim may result in a denial as a duplicate claim.
- Bill all original lines to make sure the claim isn’t rejected.
- Attach a completed Corrected Claim – Standard Cover Sheet, available under Forms on our provider website.
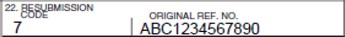
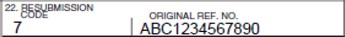
- On the CMS-1500 claim form, enter the appropriate bill frequency code in box 22, left justified in the left-hand side of the field. Use the following codes:
- 7– Replacement of prior claim
- 8– Void/cancel of prior claim
- Enter the original claim number in the “Original Ref. No.” segment of box 22:
EXAMPLE: