Corrected Claims: Including Original Claim Number is Key to Faster Processing
Some EDI corrected claims transactions are missing the correct original claim number at the point of submission. Without the original claim number that corresponds with the corrected claim, these claims must then be manually processed and sent back to the provider. This means the claim takes much longer to process to completion.
For electronic data interchange (EDI) transactions, the original claim number is sent in the REF*F8 section of the 837 claim. For EDI submissions, corrected claims will process much faster if the correct original claim number is included.
Three ways to find the original claim number
You can locate the original claim number through:
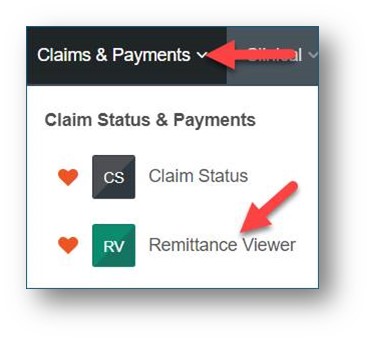
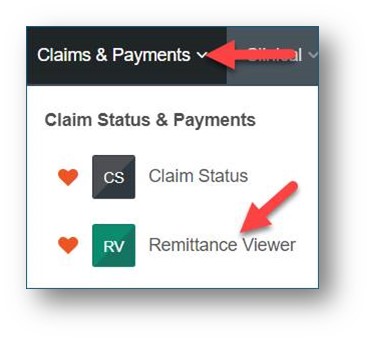
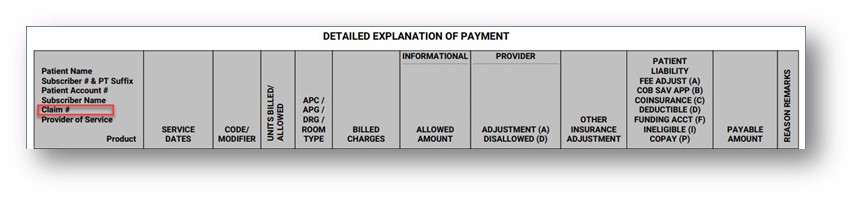
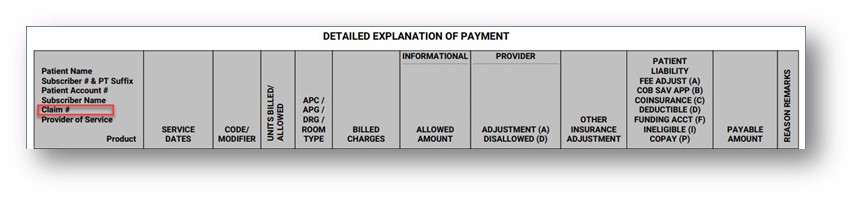
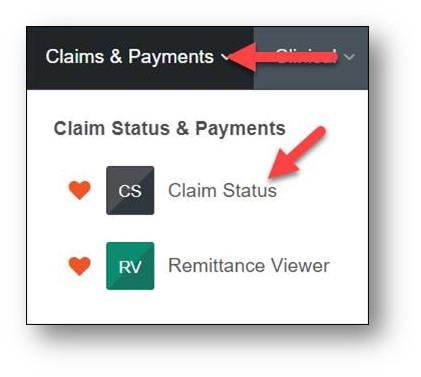
1. Availity – Explanation of Payment (EOP)
Go to Remittance Viewer and select an EOP based on the date span criteria entered.
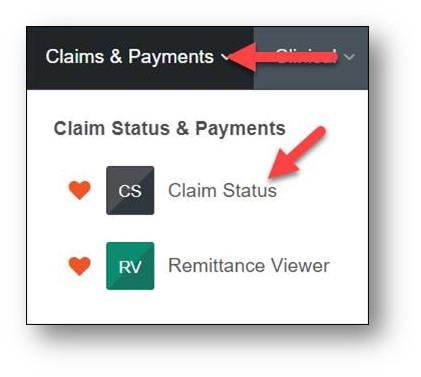
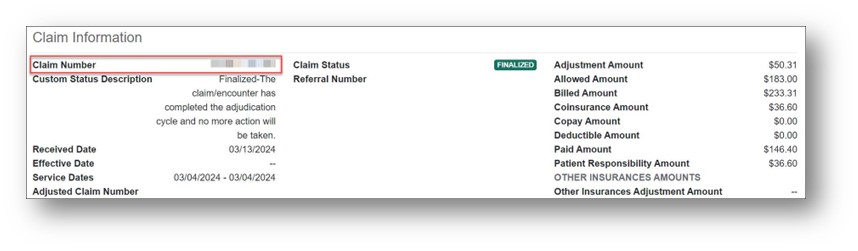
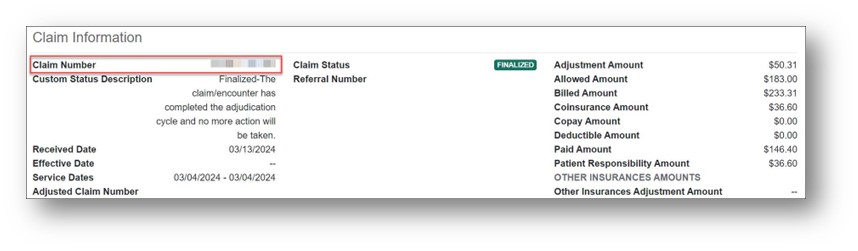
2. Availity – Claims Details
Under the Claim Status > Details screen, you can get the original claim number in the Claim Information section.
3. 835 (Electronic Remittance Advice or ERA)
Here’s an 835 example (not real data). The (bolded) Premera claim number is returned as the CLP07 value in the 835.
CLP*123456789*1*200*0**15*812345678900*02*1
More information
Visit our provider web page for more information on EDI transactions.